|
|
Post by Keelie & Bella on Jun 8, 2022 11:48:50 GMT -7
[moderator marking and removing color text. Please make a new post if there are corrections or additional info. Thanks!]☆ 1 pain? I don't believe so? Her whining I think might be due to boredom. ☐can’t find a comfortable position, appears restless: She does seem a little uncomfortable but not terribly soX Not their normal perky selves? Could definitely be due to being in her crate and not being able to move around like normal.☆2 75lbs 12 yrsA.. 300mg Gabapentin 5am, 4pm, and 9pm.
30mg Codeine 5am.
60 mg Galliprant 4pm. date of a NSAID stop?
[MED LIST/HISTORY- Moderator's Note. Please do not edit
75 lbs 12 yrs
back paws knuckling 6/2-6/6
Rimadyl without Pepcid AC!: bloody diareah/vomit; STOPPED
Galliprant as of 5/10: 60 mg 1x/day for 30 days?
Codeine 30mgs 6 or 24hrs/day
gabapentin 300mgs 3x/day
Bella needs GI tract protector, Pepcid AC, on board w/Galliprant! ☆ 4 Black Lab Bella. Keelie☆ 5 Diagnosed via xray with pinched nerve - radiologist concurred
-- DVM? YES
☆ 6 What was the date you saw the vet for CONSERVATIVE treatment? Initially saw vet about limp tail 4/7/22. Vet never recommended conservative treatment. After diagnosis 5/8, vet recommended gentle walks for strength, medication, and PT.☆ 7 bl adder control? Yes. ☆ 8 Very wobbly walking. Both back feet are now knuckling but she is able to walk properly when assisted with Help Em Up harness. Her tail has not moved since April. She is fairly unsteady.Since I was initially instructed by the vet to do gentle walks, laser therapy, meds, and look into PT, I didn't actually begin STRICT crate rest until 5/28. She was fairly quiet for most of the time beforehand, but I do now understand that her regular couch potato self probably was not helpful to her healing journey. In fact, she continued to decline and it was through my own research that I decided to do strict crate rest. I feel awful that so much time was wasted and damage done but...alas. She was getting laser treatments weekly up until a week ago but I realize might not be best for her until crate rest has ended. I do have an [⚠️]appointment with a rehab vet on 6/14 that sounds like has more knowledge and experience with IVDD but I am now wondering if I should put the appointment off until her rest time is up. Any and all help is appreciated. Thank you.
|
|
|
|
Post by Romy & Frankie on Jun 8, 2022 13:46:46 GMT -7
Welcome to Dodgerslist, Keelie. We are glad you’ve joined us all. We’ve got valuable information we’ve learned from the vets Dodgerslist consults with and our own experiences with IVDD since 2002 to share with you! Learn more about us and how we team up with veterinarians: dodgerslist.com/about-team-dodgerslist/Disc disease is not a death sentence! Struggling with quality of life questions? Re-think things:
You are doing the best thing for Bella by putting her on Very Strict crate rest. The crate rest must be very strict because when a dog walks and moves, the vertebrae move, tearing down the important scar tissue that is forming to stabilize the disc rupture. It is immobility that allows the disc to heal itself. I am not sure if you have had a chance to review the information at the link below:
Movement during potty time should also be limited. Bella is obviously too big to carry, as was my dog Frankie. What worked for me was a pee pad right outside the crate. At first, he did not want to use this. I got a paper towel with another dog's urine on it and put it on the pad. That helped him to understand the pad was an okay place to go.
You mentioned that Bella seems uncomfortable. Is she reluctant to move and restless? These are signs of pain. Not being her normal self is also a sign of pain. Bella should not be in pain because pain will slow the healing process.
Vets have many ways to treat pain. What we have seen provide the most pain relief is three pain meds on board each attacking pain differently: Methocarbamol for painful muscle contractions 3x/day. Tramadol Rx'd 3x/day as the general pain reliever Gabapentin for nerve pain also Rx'd 3x/day.
Gabapentin and Codeine alone may not be providing full relief. Have no patience with pain. If Bella seems to be in pain, let the vet know what you are seeing right away and discuss adjusting the pain meds.
When did Bella start the Galliprant? Galliprant is not commonly used for IVDD. It is mostly prescribed for arthritis. Some dogs cannot take other anti-inflammatories. This would include dogs with liver or kidney problems. In that case the vet may prescribe Galliprant.
A dog should not start PT during crate rest. There is a risk of too much movement. Dogs that are not paralyzed can get enough movement to allow for joint flexing and blood circulation by walking a very few steps to potty and moving to reposition themselves in the crate. Once crate rest is over, PT can be started.
Laser treatment can be helpful during a disc episode, but transports are always a risk to the disc of too much movement. Vet visits must be weighed risk vs. benefit. Sometimes a vet or vet tech will do home visits for laser treatments.
Are you currently giving Bella a stomach protector like Pepcid AC? This will help prevent stomach damage caused by excess stomach acid, which is a side effect of all anti-inflammatories.
It is very scary when our dogs have IVDD. It becomes less so when we learn all we can about the disease. We have more information on our main website: www.dodgerslist.com.
You can use the search bar at the top of the page to search for specific topics. |
|
|
|
Post by Keelie & Bella on Jun 8, 2022 15:01:44 GMT -7
Hello and thank you so much for your reply. Bella was initially put on Rimadyl but had bloody stool and vomit so we had to try something else. In the xrays, we found severe hip dysplasia and it honestly feels like that is how the vet has been treating Bella.
I just emailed my vet about getting Bella on the Tramadol and Methocarbamol along with the Gabapentin. Hopefully this will help.
The codeine combo seemed to help for a little bit but clearly isn't now. As for the peeing and pooping, this has been a struggle. I've been trying to figure out a way to get her to go in a specific area but she refuses. I just don't know if I would be able to get her to use a pee pad. I have been trying hard to keep her back supported when taking her out.
This has been so frustrating and incredibly disheartening since I feel like I have had no professional guidance by the one person I have been paying to do just that. I also feel like I have been failing her even when I try to do what I think I'm supposed to do. It just seems like I keep seeing her get worse and I feel so incredibly helpless.
I wanted to add that she has not been given Pepcid AC at any time. Should that be something I give her while on Galliprant?
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 8, 2022 16:47:54 GMT -7
Keelie, let me add my welcome also! Not all vets know IVDD. This means you will have to be a quick study and drive the train a bit by bringing things to the table and discuss them with your vet. The more you know the better you can help Bella. You've come to the right place to learn the right care for Bella! With x-ray, where did the vet "suspicion" the disc to be in the back: mid or lower back?What date did both back paws start to knuckle?
With new neuro diminishment hours matter with possibly getting anti-inflammatory changed..
With increased neuro diminishment, SPEAK candidly with your vet about using a more broad spectrum non-steroid or a steroid to get that swelling down. Ask if Galliprant was Rx'd specifically because Bella has heal issues that a stronger anti-inflammatory is not advisable. LEARN the difference between steroid and non-steroid anti-inflammatory drugs
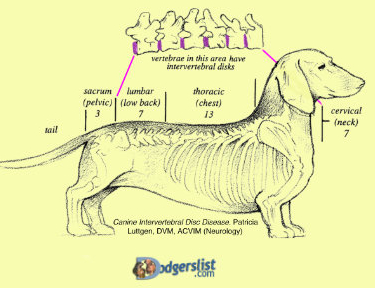
As damage to the spinal cord increases, there is a predictable stepwise deterioration of functions. When nerve healing begins, often it follows the reverse order.1. √ Pain caused by the intial disc tear & inflammation in the spinal cord2. √ Nails/toes scuffing floor
3. √ Wobbly walking, legs cross 4/7 Limp tail
4. 6/2-6 both back paws knuckle under, owner out of town
5. Weak/little leg movement, can't move up into a stand
6. Legs do not work at all (paralysis, dog is down)
7. Bladder control is lost. Leaks on you when lifted. Can no longer sniff and then pee on that old urine spot outdoors.
8. Tail wagging with joy is lost
9. Deep pain sensation, the last neuro function, a critical indicator for nerves to be able to self heal after surgery or with conservative treatment. If surgery is not an option (for whatever reason) then the best option is conservative therapy.
Surgery can still be successful in the window of 12-24 hours after loss of deep pain sensation. Even after that window of time, there can still be a good outcome. Each hour that passes decreases that chance. Precious hours can be lost with a vet who gets DPS wrong. Trust only the word of a neuro (ACVIM) or ortho (ACVS) surgeon about DPS.
A quick informative overview of conservative treatment vs. a surgery:
dodgerslist.com/2020/02/10/surgery-vs-conservative/
Would you fill in the missing detail marked in pink: MED LIST/HISTORY- 75 lbs 12 yrs Crate rest never Rx'd since 4/7! Galliprant 60 mg 1x/day for how many days?Codeine 30mgs ?x/day gabapentin 300mgs 3x/day Bella needs GI tract protector, Pepcid AC, on board w/Galliprant! First ask if Bella has any liver, kidney or heart issues. THEN l et us know when you have 30 mgs Pepcid AC on board 2x/day. Understand why: dodgerslist.com/2020/05/06/stomach-protection/
LIMITED MOVEMENT OF SPINE #1 care Read over all the potty time options. See what will work to ensure Bella is only taking a couple of FOOTSTEPS (no walking) to potty: dodgerslist.com/2022/02/10/large-dog-care-tips-ivdd/ Please keep us posted with details (date, mgs, frequency, observation details) on what the vet Rx's to adjust pain med cocktail for every 8 hrs and thoughts on switching to a stronger anti-inflammatory. NOTE: a switch from Galliprant to another anti-inflammatory WILL require: --having TWO GI tract protectors on board ( Sucralfate + the usual Pepcid AC) --Otherwise it will take 5-7 days of washout from Galliprant leaving Bella with no anti-inflammatory at all in her body. Not Good! Since you are reporting a new neuro diminishment but did not provide us with a date...so we area bit clueless if this is an emergency or not--- you will have to decide! |
|
|
|
Post by Keelie & Bella on Jun 8, 2022 17:32:00 GMT -7
Hello Paula and thank you so much for this additional information. I am incredibly grateful for yours and Romy's quick replies.
Pinched nerve is suspected to be located in the lower back.
Both back paws began knuckling over the weekend. Unfortunately, I was out of town from 6/2 - 6/6 and I noticed the change when I returned home 6/6.
Bella had her bloodwork done before meds and her panel came back beautiful, so her liver and kidneys are perfect. Unfortunately, when we tried the Rimadyl, she began to improve within 3 days but then got bloody poos and began vomiting. The Galliprant was prescribed because of that. I am definitely happy to talk with my vet though to see about a different anti-inflammatory.
Galliprant 60 mg 1x/day for 30 days (started 5/10/22)
Codeine 30mgs 6-24 hrs/day
I am going to work on a different potty area for Bella. Possibly trying to see if we can move her bed closer to the back door and/or create a little potty spot for her.
Thank you again and I will update you on what I can get from my vet.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 8, 2022 20:12:58 GMT -7
Keelie, the lower back suspicioned via an x-ray could well correlate to the L7-S1 region causing lowered tail on 4/7. X-rays show only hard tissue such as bone, but not soft tissue of disc and nerves. X-ray are use to rule out other diseases. But can't proove a disc episode location that involves discs and nerves. The neck C1-7, Chest T1-13, the low back L1-7, Sacrum S1-3 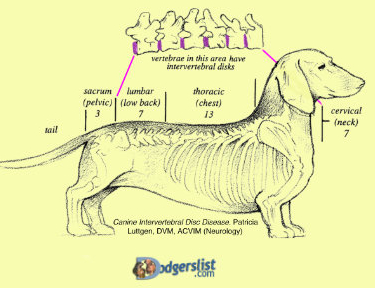 Very likely you now understand the reason for GI tract damage with Rimadyl....there was no Pepcid AC on board to suppress the extra acids. Pepcid AC with the use of any one of the anti-inflammatory drugs is necessary during a disc episode. There are some few dogs even with Pepcid AC, that have GI issues. So be aware of the progression:
lip licking of nausea> not wanting to eat> vomit> loose stool> diarrhea> bleeding stomach ulcer> red or black blood in stool> serious perforated stomach lining.
PAIN MEDS are effective for about 8 hrs.
Codeine should be promptly dosed every 8 hrs. If you've been doing every 8 hrs and still pain shows, then the codeine is not for Bella. Let us know what the vet says about traMADol (over all analgesic), methocarbamol (muscle spasm pain) and gabapentin 300mgs 3x/day (nerve pain). And what he says about Pepcid AC + sucralfate for a switch to another NSAID or even to the most powerful class the steroids such as prednisone. |
|
|
|
Post by Keelie & Bella on Jun 9, 2022 8:31:43 GMT -7
[6/9 about hour ago post]
Thank you.
I still have not heard back from the vet about the new medication. Hopefully I will hear something today. She is definitely still in pain so I will start giving her the ▲codeine every 8 hrs to see if that helps until we can get the recommended meds.
She can still get up, but with some struggle but she still refuses to use the pee pads. I have been noticing some pee dribbles when she has gotten up but nothing significant. This morning has been a struggle to get her to go pee. She pooped outside and is aggressive when I try to see if I can perhaps try to feel her bladder to see if it's full since she hasn't gone yet and it's been 10hrs since her last pee.
------
I am taking her in this morning to urgent care to get her pain managed and hopefully get some hands on guidance on expressing her bladder. Honestly I'm afraid they're going to tell me to put her down but I'm hopeful that I have the info I need from you all to help advocate for her. I will let you know what the result is.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 9, 2022 9:05:22 GMT -7
Keelie, look back up at the list of neuro function order of loss. Loss of bladder control comes AFTER loss of legs (paralyzed can no longer move legs at all). So it is unlikely she has lost bladder control. Good to get a hands on top of you hands demo just in case. FYI: A dog who has bladder control will not like having their bladder pressed on Get more out of the lesson by FIRST viewing this video to learn where, the proper pressure and where the bladder is: dodgerslist.com/2020/05/05/bladder-bowel-care/Disc disc disease is not a treatment. Stand your ground you want help with conservative treatment--- allow no talk about any nonsense killing your dog. |
|
|
|
Post by Keelie & Bella on Jun 9, 2022 13:05:23 GMT -7
UPDATE:
Went to see a different vet. Bella will now have the following medication:
- 30mg Codeine every 6-8hrs
- 300mg Gabapentin [WHICH?] 1-2 capsules every 8-12 hrs
- 500mg ✙Methocarbamol 1.5 tablets every 8-12 hrs
- 20 mg ✙Prednisone (3 day wait off Galliprant before start) 1.5 tablets/5 days. 1 tablet/10 days. 1 tablet every other day.
- 30mg ✙Prilosec 2x daily.
[MED LIST/HISTORY- Moderator's Note. Please do not edit
75 lbs 12 yrs
back paws knuckling 6/2-6/6
Rimadyl without Pepcid AC!: bloody diareah/vomit; STOPPED
Galliprant as of 5/10: 60 mg 1x/day STOPPED 6/9
✙Prednisone as of 6/12 20 mg tab: 3-day washout
30mgs 1x/day for 5 days, 6/17 test taper _pain/_neuro
Codeine 30mgs 3x/days
gabapentin 300mg tab: 600mg 3x/day
✙Methocarbamol 750mgs 3x/day
✙Prilosec as of 6/9: 30 mgs 2x/day
I asked about sucraflate and Pepcide AC and she said that she recommended just the Prilosec.
Thank you again for all of your help. I felt empowered and informed during the visit. And added bonus she never once mentioned euthanasia.
|
|
|
|
Post by Romy & Frankie on Jun 9, 2022 13:44:55 GMT -7
Good job seeing a new vet and getting a change in medication. Prednisone is a steroid type of anti-inflammatory, and therefore stronger than the NSAID type of anti-inflammatory.
Euthanasia is never an appropriate treatment for IVDD. Once Bella's pain is under control, she can heal in comfort.
A three day washout between an NSAID (Galliprant) and the prednisone is shorter than we usually see. What we see most commonly is a 5 to 7 day washout to avoid GI tract damage. When a shorter washout is needed, two stomach protectors make it much safer. An acid controller for excess acid and Sucralfate to protect any damaged areas of the stomach.
Prilosec is a good stomach protector, but it takes three to five days to reach peak efficiency. If you start to see diarrhea, particularly if it contains blood, let the vet know right away.
The change in pain meds should keep pain under control when given every 8 hours. If Bella is still showing signs of pain, let the vet know what you are seeing right away so that the meds can be adjusted.
Please let us know that Bella's pain is under control with the new meds.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 9, 2022 16:46:00 GMT -7
Keelie, good job in seeking a more knowledgeable vet to get the pain in control. It is good you were given a range in mgs and frequency. However we are in the dark to comment if we do not know what you are actually giving. Please fill us in on what is actually given: Prednisone 20mg tab: 30mgs ?x/day for 5 days, then date? of taperGabapentin 300mg tab: ?mg ?x/day
methocarbamol 500mg tab: 750mg ?x/day
Codeine 30mgs ?x/day
COMMENTS: Prednisone was Rx for a 5-day course. What is the date of the first dose 30mg dose 2x/day?
The taper date will be the time be alert for pain. If pain the vet will know another Pred course is needed.
Pain meds are typically also stopped so you have no blind fold on about the status of pain. Rule of thumb on a taper:
pain = swelling =
back up at original anti-inflammatory pred dose +
pain meds + Prilosec Pepcid AC & Sucralfate is used when deemed an emergency to save nerve damage with NO DAYS of washout. Emergency means to immediately dose prednisone AND have both GI protectors on board. You and your urgent/ER vet deemed the switch was not of an emergency nature. Therefore taking time with a 3-day washout before switching to Pred. With no anti-inflammatory on board for 3 days, one would expect pain to escalate and need compensation with increase of pain meds. Since you've been given an every 8 hrs (3x/day) option, would be a good idea to give all pain meds PROMPTLY 3x/day (codeine, gabapentin, and methocarbamol) Prilosec. As you've read and Romy underscored, Prilosec take 3-5 days to reach peak effectiveness. Let us know you are giving Prilosec as of today 6/9. Will be watching for your update on pain status and to know with 3-day Galliprant washout, pain meds are doing the job dose to dose, round the clock. Also keep a watchful eye on any new or increased neuro diminishment while Galliprant is being given. If you see setback (emergency) immediately alert the vet. Advocate for Pepcid AC & sucralfate and immediate start of Prednisone. Unfortunately the washout days happen over the weekend when the vet is not open?? If this was ER vet, any other vet on duty can read Bella's folder and adjust meds, prescribe over the phone. Transporting a large dog is a risk of too much movement when things can be handled over the phone. |
|
|
|
Post by Keelie & Bella on Jun 10, 2022 16:30:06 GMT -7
I have the added info below. It has been stressful to say the least and I am also battling being sick myself.
Her pain seems to be slightly better but I am noticing that the lack of anti-inflammatory seems to have amped [pain] it up slightly so I'm making sure that she is on a set schedule with all meds and consistent.
Prednisone (Will begin 6/12) 20mg tab: 30mgs 1x/day for 5 days, then 6/17 of taper
Gabapentin 300mg tab: 600mg 3x/day
methocarbamol 500mg tab: 750mg 3x/day
Codeine 30mgs 3x/day
We will start [prednisone] 6/12
Yes I started giving her Prilosec as of 6/9.
Thankfully my vet is open on the weekends so I can still get in touch if need be.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 10, 2022 19:28:21 GMT -7
Keelie, you can help us. We only want to read your words in your post. It is confusing to see quotes from us in your reply.
Use the "QUICK REPLY" area down at the bottom of the page to write your replies. Use 1-2 of our words if that helps to explain, then finish off your thought in a full sentence. QUICK REPLY allows you to scroll up to read a post and back down to finish writing your reply. Thanks!
Finished marking up your post and now reading and forming reply to you.
Refresh your browser to see my post.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 10, 2022 19:35:40 GMT -7
Keelie, I'm so sorry to hear you are not well. Your excellent efforts in caring for your girl are even more awesome!
Very good your vet is open weekends. Does that include Sunday?
Fingers crossed you will get a good nights sleep as hopefully Bella will with pain in control. Keep us posted over the weekend. Hope to hear all is going well.
|
|
|
|
Post by Keelie & Bella on Jun 11, 2022 11:43:28 GMT -7
Eep! Yes, I will do that! I've been responding on my phone and it doesn't give the Quick Reply option.
Bella appears to be more comfortable. Some panting, some whining, but I can't tell if it's out of pain or just boredom or even a side effect from all the meds. She does seem more weak in her hind end but the vet had said that would happen with the medication. She is going potty normally but we are still trying to get her to go without taking us on an adventure. This has been the most challenging part I think.
We begin the Prednisone tomorrow 6/12, so I will update on how she is doing then. We have been giving her Prilosec 2x/day since 6/9 so hopefully that will be enough time to take effect.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 11, 2022 12:09:06 GMT -7
If hard to decide if pain, observe if there are two or more signs of pain to confirm pain vs. anxiety, being cold, being too hot. Do the signs surface nearing next dose of pain meds or when have to move, then likely "pain"
SIGNS OF PAIN: ⚙︎ shivering-trembling ⚙︎ yelping when picked up or moved ⚙︎ tight tense tummy ⚙︎ arched back, ears pinned bac ⚙︎ restless, can't find a comfortable position ⚙︎ slow or reluctant to move in suite such as shift positions ⚙︎ not their normal perky interested in life selves
Weakness in hind end can be neuro diminishment OR pain meds making leg control wobbly, weak. If determined actual new or increased neuro diminishment such as slow to right paw now... can't right paw at all- hours matter in getting prednisone on board.
If shorting the washout days, then TWO protectors need to be on board: Rx item sucralfate + prilosec Each works in a different way to protect the GI tract.
As damage to the spinal cord increases, there is a predictable stepwise deterioration of functions
1. Pain caused by the intial disc tear & inflammation in the spinal cord
2. Wobbly walking, legs cross
3. Nails/toes scuffing floor
4. new on 6/2-6 Both paws knuckle under (slow to right or can't right at all?)
5. Weak/little leg movement, can't move up into a stand
6. Legs do not work at all (paralysis, dog is down)
7. Bladder control is lost. Leaks on you when lifted. Can no longer sniff and then pee on that old urine spot outdoors.
8. Tail wagging with joy is lost
9. Deep pain sensation, the last neuro function, a critical indicator for nerves to be able to self heal after surgery or with conservative treatment.
|
|
|
|
Post by Keelie & Bella on Jun 11, 2022 14:42:52 GMT -7
Both of Bella's back paws do not self correct when knuckled.
However with assisted walking she will go back and forth between knuckle walking and normal walking.
|
|
|
|
Post by Romy & Frankie on Jun 11, 2022 15:03:36 GMT -7
With the knuckling, which is caused by nerve damage, it is really good that the pred is starting tomorrow.
Are you seeing any signs of pain now?
|
|
|
|
Post by Keelie & Bella on Jun 11, 2022 16:50:31 GMT -7
Not that I can tell. She has been panting a little bit and whining off and on but I don't think it's from pain. She doesn't appear uncomfortable. The vet did call to see how she was doing and said that the panting could be from her meds.
From what I understand from the readings, do I still give her all the pain meds UNTIL the tapering of the Prednisone? Also, do I continue Prilosec throughout Prednisone?
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 11, 2022 19:44:22 GMT -7
Keelie, how nice of your vet to phone for an update on Bella!
If you are like me, knowing the why behind things helps to be committed to care, helps to advocate on behalf of our dogs if need be.
PAIN MEDS either stop or start backing off (via several days) on the day pred tapering begins. Which does your vet want on Fri. June 17?
The beginning of the pred taper is the time to observe for pain signs surfacing.
PREDNISONE is used until all painful spinal cord swelling is gone.
All anti-inflammatory drugs can have serious side effects. No one wants to use any anti-inflammatory drug one bit past the point all painful swelling has been, in Bella's case, fully resolved by prednisone.
A vet must simply take a guess on how many days that might take. Often the guess is a 5-7 days course of pred.
The taper day is the time to be alert to assessing pain. Pain meds on board on the day the taper starts deters you from your job. Your job is to quickly as possible be allowed to see any hint pain. If you do see pain surface, alert the vet on the signs you see so another course of pred, another taper can be tried.
Typical is in the range of 7 to 30 days for pred to do its job. Taper days are not at an effective level to work on swelling. Taper days do not count in the 7-30 days.
PRILOSEC once at an effective level in about 3-5 days, is an excellent acid suppressor.
As you've read there are several factors that could contribute to extra stomach acids being produced. Prilosec's job is to suppress stomach acid production and avoid bleeding ulcers for the duration of prednisone use.
#1 Anti-inflammatory drugs are known to increase stomach acids production
#2 Stress increases stomach acid production just as in people who experience ulcers! Change is routine is a big stressor for dogs who LOVE the routine. Resting in a recovery suite is a big change.
#3 Spinal cord damage can inhibit an involuntary function protecting the stomach lining.
|
|
|
|
Post by Keelie & Bella on Jun 12, 2022 19:54:26 GMT -7
UPDATE: Bella started Prednisone [6/12] today and seems to be doing well. She is definitely super sedate but definitely not in pain now and all panting and whining seems to have abated. Peeing has increased but not by a ton but I suspect it will increase soon. She also seems more picky about eating her meals. Still eager to have treats but her regular meals she turns her nose up. I found putting her kibble in kongs with peanut butter she is much happier with.
I am hoping that she will be more willing to use the pee pads when having to go more more frequently.
So it looks like I do 1.5 pills of Pred for 5 days then (6/17)1 pill 10 days - I assume this is then when I discontinue the pain meds to see how her pain is. Correct?
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 13, 2022 7:55:47 GMT -7
Prednisone as of 6/12 20 mg tab: 30mgs 1x/day for 5 days, 6/17 test taper _pain/_neuro
"PAIN MEDS are either stopped or start backing off (via several days) on the day pred tapering begins. Which does your vet want on Fri. June 17?
The beginning of the pred taper is the time to observe for pain signs surfacing."
Did not see the answer to what your vet wanted in your lasts posts.
If your vet has directed a full stop of all pain meds, then all pain meds are cold turkey stopped on Fri. June 17th to allow you to quickly observe if any painful inflammation still exists.
|
|
|
|
Post by Keelie & Bella on Jun 14, 2022 21:12:16 GMT -7
I finally heard back from vet about pain meds with pred taper and they said to continue all pain meds as directed.
Should I consider cutting her pain meds in half? I know the point is to determine whether or not inflammation is down.
She seems comfortable if not a little board. Definitely a little lethargic. Slightly more stable on her feet when going potty but I don't want to be too hopeful since I know pred can give a false sense of hope. We are continuing as before frankly.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 15, 2022 8:53:09 GMT -7
Keelie, you will have to determine your sense about the comfort level your vet has with IVDD basing it on prior treatments with this disc episode. "This means you will have to be a quick study and drive the train a bit by bringing things to the table and discuss them with your vet." This means to also question the thinking behind prescribed treatments. Your ability to understand, means you see if it makes sense or ability to inquire more or suggest another approach.
• "continue all pain meds as directed" Does not indicate the reason behind the treatment but confirms to follow directions on the bottle. QUESTION: What is the harm to either full stop meds or to begin backing them down at the begin of the taper?
Codeine 30mgs 3x/day (no Rx lower than currently being given)
gabapentin 300mg tab: 600mg 3x/day (Rx'd 1-2 capsules every 8 or 12 hrs)
Methocarbamol 750mgs 3x/day (Rx'd 1.5 tabs every 8 or 12 hrs)
If you will be following the directions on the bottle, please confirm your adjustments so we can follow along with accurate info (date of adjustment, mgs, frequency) for each pain med.
With any adjustment in meds, please update us on your observations of both pain level and any new or increased diminishment of nerve function.
Last observation was:
|
|
|
|
Post by Keelie & Bella on Jun 19, 2022 11:34:49 GMT -7
Vet has recommended that we finish out bottle of pred with last tapering being 1 tablet every other day. We will continue all other meds at current level and will wait 1-2 weeks after Pred is finished. If Bella seems good, then we will begin tapering off the codeine (no instructions yet for that).
[MED LIST/HISTORY- Moderator's Note. Please do not edit
75 lbs 12 yrs
back paws knuckling 6/2-6/6
Rimadyl without Pepcid AC!: bloody diareah/vomit; STOPPED
Galliprant as of 5/10: 60 mg 1x/day STOPPED 6/9
Prednisone as of 6/12: 20 mg tab: 3-day washout
30mgs 1x/day for 5 days, 6/17 test taper _pain/_neuro
Codeine 30mgs 3x/days (wait 1-2 wks after last dose of pred to stop)
gabapentin 300mg tab: 600mg 3x/day (no instruction to stop or back off on taper)
Methocarbamol 750mgs 3x/day (no instruction to stop or back off on taper)
Prilosec as of 6/9: 30 mgs 2x/day
UPDATE ON BELLA: We started pred tapering to 1 [20mg] tablet for 10 days. Yesterday she actually seemed a little like her old self. She seemed interested in what we were doing, a little playful, and wanted to get up and move a little (which we didn't allow). Today she seems a little more sedate again but it was nice seeing her old personality back.
She is still exhibiting [nerve damage] wobbly and unsteady walking. Not a lot of changes there. Yesterday she was able to stand by herself for a hot minute in her rest area without assistance.
I have noticed that she is not peeing very frequently and tends to hold her urine for longer periods of time. I have an email to the vet in about this but wasn't sure if this is something that is common with IVDD. When she goes, it's a strong stream with no visual blood. She also doesn't seem as thirsty as I was expecting with with Prednisone.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 19, 2022 17:08:55 GMT -7
Keelie, nice to hear Bella is acting like her old self with the taper of pred. Pred can cause personality changes for some dogs.
As long as Bella is not being rambunctious in her recovery suite, there is no reason she can't get up to stand, turn around, sit, etc. The limited area is enough limit when a dog is calm to have a bit of movement of legs when repositioning or standing to see what's going on around the home.
Not all UTI's will have observable signs. Will be interested in what your vet's take is on holding urine. How often does she go potty...every ? hours?
|
|
|
|
Post by Keelie & Bella on Jun 19, 2022 21:06:37 GMT -7
Bella is definitely not being rambunctious. She has always been a bit of a couch potato so the hardest thing was creating a space where she was no longer allowed to climb up on the couch. She did not like that. lol!
I did hear back from the vet and she said that if Bella was not straining and didn't look in pain/uncomfortable that she should be fine.
Of course, at about 4pm she also started peeing outside every 2 hours making me feel like I was a worrywort. I'm thinking that she hasn't been drinking as much water at night and she has been pretty sedate in the morning through the afternoon. I will continue to monitor but I won't try to worry too much.
Is it common for dogs tapering off pred to have good days and meh days? Just curious since she had seemed so good yesterday but was pretty quiet and sedate again today.
|
|
|
|
Post by Keelie & Bella on Jun 20, 2022 5:27:59 GMT -7
Bella did not have a good night. She was barking and panting and wanting to go potty but when we took her she growled several times (not at us) and at one time she yelped. I'm assuming that she is in pain and we need to go back up on the pred.
I have given her her original 1.5 tablet of ▲pred 6/20 this morning and will be letting the vet know that we might need to push back the taper.
[MED LIST/HISTORY- Moderator's Note. Please do not edit
75 lbs 12 yrs
back paws knuckling 6/2-6/6
Rimadyl without Pepcid AC!: bloody diareah/vomit; STOPPED
Galliprant as of 5/10: 60 mg 1x/day STOPPED 6/9
Prednisone as of 6/12: 20 mg tab: 3-day washout
30mgs 1x/day for 5 days, 6/17 test taper √6/19 pain/_neuro
as of 6/20: 30mgs 1x/day for 5 days, 6/25 test taper _pain/_neuro
Codeine 30mgs 3x/days (wait 1-2 wks after last dose of pred to stop)
gabapentin 300mg tab: 600mg 3x/day (no instruction to stop or back off on taper)
Methocarbamol 750mgs 3x/day (no instruction to stop or back off on taper)
Prilosec as of 6/9: 30 mgs 2x/day
[Posted 6/19:]
Bella is definitely not being rambunctious. She has always been a bit of a couch potato so the hardest thing was creating a space where she was no longer allowed to climb up on the couch. She did not like that. lol!
I did hear back from the vet and she said that if Bella was not straining and didn't look in pain/uncomfortable that she should be fine.
Of course, at about 4pm she also started peeing outside every 2 hours making me feel like I was a worrywort. I'm thinking that she hasn't been drinking as much water at night and she has been pretty sedate in the morning through the afternoon. I will continue to monitor but I won't try to worry too much.
Is it common for dogs tapering off pred to have good days and meh days? Just curious since she had seemed so good yesterday but was pretty quiet and sedate again today.
|
|
PaulaM
Moderator.    Member since 2007: surgery, conservative . Montana, USA
Member since 2007: surgery, conservative . Montana, USA
Posts: 19,928
|
Post by PaulaM on Jun 20, 2022 10:17:40 GMT -7
Keelie, I’m sorry you are having difficulties identifying pain.
The usual on a prednisone taper is to remove all distractions. Some pain meds can have side effects that might appear to be pain or like function related. Of course, since you are single minded In looking for signs of pain or new neural diminishment, observations could be skewed to lean to actual pain or actual neuro diminishment.
On the next prednisone taper, advocate for all Pain meds (Gabapentin, codeine, and methocarbamol) To be either full stopped on the date prednisone taper starts or begin backing off in Meigs dose and frequency.
Let us know for how many days your vet will want Bella on the anti-inflammatory level of prednisone (30mgs 1x/day.)
|
|
|
|
Post by Keelie & Bella on Jun 30, 2022 20:10:22 GMT -7
Update on Bella:
We began tapering prednisone 6/25 to 20mg for 10 days. After a 2nd discussion with the vet, she recommended again that we stay on the pain meds and then taper them off after the pred taper.
[MED LIST/HISTORY- Moderator's Note. Please do not edit
75 lbs 12 yrs
back paws knuckling 6/2-6/6
Rimadyl without Pepcid AC!: bloody diareah/vomit; STOPPED
Galliprant as of 5/10: 60 mg 1x/day STOPPED 6/9
Prednisone as of 6/12: 30mgs 1x/day for 5 days, 6/17 test taper √6/19 pain/_neuro
as of 6/20: 30mgs 1x/day for 5 days, 6/25 test taper _pain/_neuro
Codeine 30mgs 3x/days (wait 1-2 wks after last dose of pred to stop)
gabapentin 300mg tab: 600mg 3x/day (no instruction to stop or back off on taper)
Methocarbamol 750mgs 3x/day (no instruction to stop or back off on taper)
Prilosec 30 mgs 2x/day
However, as of today, we are currently in communication since Bella [6/30]has developed sudden bladder control issues/incontinence that could potentially be due to her meds. Bella's mobility has not changed but she has gotten weaker in her back end since starting the meds. I now have to help her poop even though she can walk with assistance and move her legs but is weak, wobbly, and still knuckles both back feet.
In addition, Bella developed a UTI and is being treated with an antibiotic [name; mgs; x/day]for that.
Bella is not showing any negative side effects to a pred taper that would suggest pain/inflammation. She is beginning to whine in the evening and show some restlessness, which the vet thinks could be due to the lower dose of pred. I have started giving her about 50-100mg of Trazadone in the evening to help keep her comfortable.
All in all, she appears comfortable, if not a little anxious which hopefully will be addressed with the Trazodone.
|
|